 Rosie is currently a final year student at Barts and the London. During her fourth year she went on an Erasmus Exchange to the Karolinska Institute in Sweden for three months. Rosie says, "Whilst there, I was able to treat patients and it was a good experience to both practise dentistry and to live in another country."
Rosie is currently a final year student at Barts and the London. During her fourth year she went on an Erasmus Exchange to the Karolinska Institute in Sweden for three months. Rosie says, "Whilst there, I was able to treat patients and it was a good experience to both practise dentistry and to live in another country."
"Talking to friends when I returned to London, I found that a lot of them were interested to learn more about CAD/CAM and my experience of using it. It's not currently taught within our curriculum, so we haven't much exposure to learning about digital dentistry. Therefore, I decided to write the article hopefully to be of interest to dental students and provide a starting point for them to find out more about the technology."
Introduction
Within the undergraduate curriculum at the Karolinska Institute, Stockholm the use of a CAD/CAM (computer-aided design/computer-aided manufacturing) CEREC (Ceramic Reconstruction) system is taught alongside conventional indirect restorative methods. The use of CAD/CAM for in-surgery manufacture of crowns and other prosthodontics is making an appearance in private practice across the UK, due to its speed and apparent ease of use. However, traditional methods are still widely used and it is these that are usually taught to the majority of undergraduate dental students. This article aims to describe the practicalities of using digital dental technology in providing treatment for a patient at undergraduate level.
Towards the end of my fourth year at Barts and the London, I had the opportunity to spend three months at the Karolinska Institute, Stockholm, a University known for its research and affiliation with the Nobel Prize. As a person who usually favours hot climates it was slightly daunting arriving in January to a thick layer of snow and short daylight hours. The dental school is similar to the open plan style clinics usually seen in UK dental schools and well accustomed to a fairly large number of exchange students arriving at different points throughout the year. A separate list of English-speaking patients is set aside for exchange students and therefore I had my own patient list to keep me busy throughout my time there.
Although similar to London, one significant difference is the use of a CAD/CAM (computer-aided design/computer-aided manufacturing) CEREC system alongside conventional indirect restorative techniques. CAD/CAM technology utilizes digital design to fabricate indirect ceramic restorations which can be milled on-site in under ten minutes, significantly reducing treatment time. These systems were introduced in the 1970s[i] and have been increasing in popularity since then. One major criticism of CAD/CAM indirect restorations is the marginal fit, which is believed to be less accurate than conventional methods. However, this is mainly relevant to earlier machines as current studies report marginal discrepancies of less than 50µm, within the 100µm clinically acceptable range.[ii],[iii]
My Patient
The Sirona CEREC MC XL system was purchased by the Karolinska Institute in 2011. Initially, the clinical tutors spent six months learning how to use the system ready for incorporation into the curriculum. Theoretical teaching takes place towards the end of third year, ready for use on clinic by the start of fourth year. Whilst at the Karolinska Institute I had the opportunity to provide a CEREC onlay for a patient to restore the 37 which had a large occlusal composite and fractured distolingual cusp (Figure 1). 37 was the last remaining lower molar tooth, the 14 and 26 had been previously extracted. The patient was medically fit and well, with no allergies and taking Pregabalin for anxiety. The patient did not smoke or drink alcohol. Oral hygiene was good but caries risk was increased due to medication-induced xerostomia.

The 37 was not root canal treated nor symptomatic, sensibility testing was positive and pre-operative radiographs showed no periapical radiolucency. Case selection is important as a fairly destructive shoulder preparation is required; in this case much of the tooth tissue had already been replaced with composite. It is important to have a clear shoulder margin of at least 1mm for accurate CEREC camera detection and optimum porcelain strength in this area.[iv] The tooth was prepared using a round-end tapered diamond bur with supragingival margins located in enamel (Figure 2). As with any all-ceramic restoration, sharp angles should be rounded to reduce the chance of fracture via stress concentration.[v] Shade selection was also performed at this stage. In practice, the tooth preparation can be scanned intraorally however, at the Karolinska Institute, students take impressions and scan a Fuji rock model (Figure 3). This provides impression-taking and temporary crown fabrication experience as well as avoiding problems on clinic of machine availability. An upper impression needs to be taken as this is also scanned, allowing occlusal configuration.
The software allows simple design of a restoration based on a generic database or by making a copy of the contralateral tooth. The occlusion and thickness of the ceramic is adjusted virtually. This stage provides an appreciation of tooth morphology and principles of occlusion for undergraduate learning. After design, the onlay was milled from a shade-specific pre-fabricated block of ceramic (IPS e.max CAD blocks) to produce a 'blue' stage restoration (Figure 4). This blue stage is a precrystallised intermediate-strength phase which allows adjustments to be made before final strength is achieved after sintering.[vi] The onlay was tried-in during a second appointment to check margins and occlusion. There was a good marginal fit but the occlusion needed to be adjusted slightly. After try-in the restoration is glazed and can be characterised by painting on various stains of brown, blue and white according to a shade guide.[iii]

Once glazed, the onlay is placed in a ceramic furnace (Ivoclar Vivadent Programat® CS) where it reaches a crystallisation temperature of 840°C and final compressive and flexural strength of 360MPa.[iii] Conventional amalgam and hybrid composites have a compressive strength of around 300MPa.[vii] This stage took 25 minutes, plus time needed for glaze and surface characterisation (Figure 5). Appointments at the Karolinska Institute are three hours long, so I was able to complete sintering, characterisation and cementation within one appointment. One option for dental practices is to send the data of their scanned preparation to a dental laboratory which can then design and mill the restoration, ready for placement at a second appointment. For dental practices that invest in a milling machine and furnace, ceramic blocks requiring a shorter firing cycle can be used. In combination with direct intra-oral scanning, rather than taking impressions, one-visit preparation and placement is achievable.
The fit surface of the onlay was etched with 5% hydrofluoric acid for 20 seconds and a neutralising powder applied for 5 minutes. Multilink® Automix bond system was used which is a resin-based dual-cure adhesive.[viii] The onlay preparation was etched with 37% phosphoric acid, washed and dried before bonding. Multilink® bond, primer and automix were applied, the restoration seated and held in place firmly. The margins were cured for 5 seconds and excess cement was easily removed using a hand scaler, before curing for a further 20 seconds. The restoration was polished to smooth any remaining excess cement and occlusal contacts and marginal fit checked. The patient was very happy with the appearance of the onlay (Figure 6).

When the CAD/CAM CEREC course was introduced into the Karolinska curriculum, practical learning of diagnostic wax-ups was removed due to timetable restrictions. Students receive three hours of lectures about CAD/CAM design followed by three pre-clinical sessions in the laboratory. The preclinical sessions cover all stages of providing a CEREC crown, from preparing a lower molar tooth, to scanning, design and cementing. Luckily, I was able to work closely with the clinical tutors whilst carrying out CEREC treatment, to help me with the different stages of scanning, design and placement. Not all students in fourth year had yet treated a patient using a CEREC restoration, however, they appreciated the course and saw it as valuable for their future work.

Summary
The system has allowed the production of highly aesthetic restorations which can be placed within one appointment. This convenience for both patients and practitioners will likely drive increased availability and demand for CAD/CAM systems within the UK. In the future this may need to be more widely incorporated into UK dental school teaching to equip undergraduates with the skills and knowledge to deliver modern aesthetic and conservative restorative treatment.
Rosie Pritchett
[email protected]
Figure 1 Study models of the patient's upper and lower dentition, showing partially dentate upper and lower arch and broken down 37.
Figure 2 Occlusal and lingual view of tooth preparation for CEREC onlay 37, showing shoulder preparation and occlusal reduction. Buccal concavity due to removal of a previous buccal amalgam restoration.
Figure 3 Scanning the model using the Sirona CEREC MC XL system. Photo on the right shows the onlay design showing occlusal contacts, blue indicates light contacts, progressing from green to yellow to red, indicating progressively heavier contacts. Upper and lower models are scanned separately and then a buccal scan is taken with the models in occlusion.
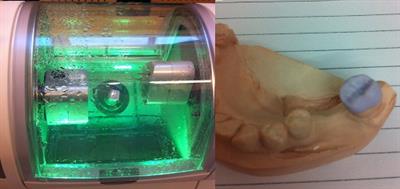
Figure 4 Sirona CEREC MC XL 3-axis milling unit at start of onlay fabrication. Photo on the right shows 'blue' stage onlay which can then be tried-in to assess marginal fit and occlusion.
Figure 5 Table-top Ivoclar Vivadent ceramic furnace Programat® CS and onlay after sintering; opaque white stains were used for cusp tips and darker stains for occlusal characterisation.
Figure 6 Finished onlay showing good colour match and aesthetics. Photo on the right shows the tooth in occlusion, note presence of upper temporary acrylic denture replacing 14 and 26 whilst patient was waiting for an implant assessment.
[i] Chatham C, et al. (2014) The introduction of digital dental technology into BDS curricula. BDJ;217:639-642.
[ii] Hamza TA, Ezzat HA, El-Hossary MMK et al. (2013) Accuracy of ceramic restorations made with two CAD/CAM systems. J Prosthet Dent;109:83-87.
[iii] Mjör IA, Davis ME, Abu-Hanna A. (2008) CAD/CAM restorations and secondary caries: a literature review with illustrations. Dent Update;35:118-120.
[v] Shillingburg HT, Sather DA, Wilson EL et al. (2012) Fundamentals of fixed prosthodontics, 4th edition, USA: Quintessence Publishing Co, Inc.
[vi] Poticny DJ, Klim, J. (2010) CAM/CAM in-office technology: Innovations after 25 years for predictable, esthetic outcomes. JADA;141:5S-9S.
[vii] McCabe JF, Walls AWG. (2008) Applied dental materials, 9th edition, UK: Blackwell Publishing Ltd.